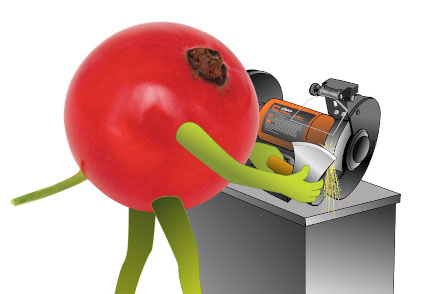
The idiom “to have an axe to grind” means to have a selfish reason or strong opinion that shapes one’s actions. The idiom’s origin is apparently based on an 1811 story titled “Who’ll Turn the Grindstone?”, in which author Charles Miner recalls being a little boy and meeting a man with an axe. The man praised Charles as a “fine little fellow,” then asked him if his father had a grindstone he could use to sharpen his axe. Charles offered the man his father’s grindstone. Flattered by the man saying “you are one of the finest lads” he ever saw, the boy worked on the axe. The school bell rang but the axe was only half ground; with blistered hands and exhaustion, the boy kept working until the task was done. The man then scolded Charles for being late to school and called him a “little rascal” and a “truant.” Charles never forgot the hurtful incident, and whenever he saw a person calling on support for their personal gain, he’d assume they had “an axe to grind.”
Today, there is a group of individuals who clearly have their own axes to grind. These pro-pharma market access, pricing and reimbursement, and health policy analysts never saw a drug they didn’t like, a drug priced too high or whose patent protection lasted too long, or appropriate utilization management (e.g., step therapy, prior authorization, exclusion). They obsessively criticize (sometimes fairly) a triad of issues — PBMs, the Inflation Reduction Act (IRA), and the 340B program but are never critical of drug manufacturers.
Recent examples of bias
It is easy to spot analyses and reports of those who have an axe to grind.
The first installment of an IQVIA report, “The Cost of the 340B Program,” released on March 12, 2024, estimated that the drug pricing program costs self-insured employers and their workers $5.2B per year in lost rebates. Many quickly and publicly embraced the results without question — confirmation bias likely blunted their skepticism. In a critique of IQVIA’s analysis, Currant identified many reasons the sensational result was likely wrong, while simultaneously acknowledging how the IQVIA model may still be useful. The National Pharmaceutical Council (NPC) funded IQVIA’s analysis and provided feedback on the manuscript. It would be naïve to think the NPC’s pro-pharma agenda did not shape IQVIA’s analysis.
On June 21, 2024, the New York Times published “The Opaque Industry Secretly Inflating Prices for Prescription Drugs,” a front-page article that was highly critical of PBMs. Without reservation, pro-pharma analysts embraced this “exposé” of one of their favorite targets. But look more carefully, and it becomes clear that the language or framing used by the Times was biased. Right out of the gate, the Times used the pejorative term “middlemen” to stoke disdain. The Times noted how “when clients do the math, many [emphasis added] are realizing that the expected savings don’t exist” — a clever way to avoid stating, falsely, that savings don’t exist. It was intentionally inflammatory in highlighting a quote that described PBMs as the “arsonist and firefighter of high drug prices.”
This is not to suggest that the Times has been co-opted by pharma; it has done some excellent health care reporting. But this article ignored the value PBMs add. Repeatedly suggesting that PBMs drive up costs grinds against the evidence sophisticated employers and benefit consultants have of PBMs cutting costs. Saying that “PBMs sometimes [emphasis added] push patients toward drugs with higher out-of-pocket costs, shunning cheaper alternatives” ignores when patients are incented or required to use drugs with lower out-of-pocket (OOP) costs. Noting how “PBMs sometimes [emphasis added] delay or even prevent patients from getting their prescriptions” is accurate, but adding “in the worst cases, patients suffer serious health consequences” is cherry picking. Saying that PBMs are “driving up drug costs for millions of people, employers and the government,” is overly simplistic.
On June 24, 2024, Milliman released a report commissioned by Pharmaceutical Research and Manufacturers of America (PhRMA) titled “Expected Impact of Inflation Reduction Act (IRA) Medicare Drug Price Negotiation Program on Medicare Part D Beneficiary Out-of-Pocket Costs.” The analysis appears to be rigorous, but the spin is misleading. The PhRMA press release focuses on the “bad” news — how approximately 3.5 million Medicare beneficiaries who use drugs selected for price negotiation will face higher OOP costs (an increase of approximately $70). For context, it is important to note that the Medicare Part D program provides an outpatient prescription drug benefit to more than 50 million Medicare beneficiaries. The PhRMA press release conveniently ignores how the Milliman report estimates that nearly an equal number of beneficiaries using drugs selected for price negotiations will either experience no change in OOP costs or will realize cost savings. The Milliman analysis focuses on the incremental impact drug-price negotiations after implementation of the 2024 Part D benefit redesign and does not bother to quantify the many more millions of beneficiaries who, thanks to the IRA, have lower OOP costs through:
- The $2,000 annual cost cap on Part D drugs
- The $35 monthly cost cap on insulin
- The free vaccines
- The expanded eligibility for full Part D Low-Income Subsidies, thereby eliminating OOP costs for more beneficiaries
In its press release, PhRMA quoted its president and CEO, Stephen J. Ubl, as saying, “This report is further evidence the IRA’s new drug pricing scheme will have significant unintended consequences for millions of Medicare Part D patients.” While factually true, the quote focuses on a very a small piece of the story and, as a result, is misleading. And using the pejorative term “scheme” was likely intentional for effect.
Bias explained
Unaided, if you ask pharma industry observers within and without pharma who are some of the most biased pro-pharma analysts, a short list of frequently cited individuals emerges. And if you ask those industry observers about any analyst on that short list, they will confirm the bias. They won’t say, “I don’t know them from Adam.”
The emergence of biased, pro-pharma analysts is not surprising. Some of this is explained by confirmation bias where people search for, interpret, favor, and recall information that confirms or strengthens their beliefs or values. But the pharma industry and its trade organizations predictably commission, influence, promote, and spin reports in ways that advance their public relations, legal, and lobbying efforts aligned with their vested financial, political, and reputational interests. Some entrepreneurial analysts respond to pharma’s demand for and support of biased insights due to the economic and social rewards. Over time and with practice, their own beliefs and values may shift and become aligned with a pro-pharma bias.
The hazards of bias
Embracing biased insights is as hazardous as wielding a dull axe — it may cut, but not where intended. Biased insights may result in an incomplete understanding and suboptimal and possibly counterproductive decisions, including a misallocation of resources and a slowed response to changing market dynamics. Flawed beliefs and values may become entrenched and dysfunctional. And an echo chamber reinforcing mistrust and an adversarial, polarizing us-versus-them mentality can get in the way of the partnerships and collaboration needed for creative solutions and innovative approaches (e.g., value-based contracts).
Promoting biased insights or spinning objective insights could (and should) result in a loss of credibility and an erosion of trust.
Ways to reduce bias
Pharma and other stakeholders should critically review all insights, especially those commissioned and/or promoted by PhRMA, NPC, or other organizations with clear advocacy agendas. And insights that fail to consider a diversity of views, scan for conflicting evidence, or explore alternative hypotheses should be viewed with skepticism. Peer review and replication studies can also help reduce bias.
Social media can be used to help spot bias. For example, if the vast majority of a post’s likes, comments, and reposts on LinkedIn are from pharma and/or pro-pharma analysts, then the content is likely aligned with their beliefs or values. This does not necessarily mean the content is biased, but there is a good chance that confirmation bias may be at play. Social media can be used to call out bias when it is blatantly obvious. But social media’s algorithms may, unfortunately, reinforce bias by displaying content in feeds predicted to be of interest to a viewer.
Hone in on the truth. Have an axe to grind with those who have an axe to grind.


No Comments